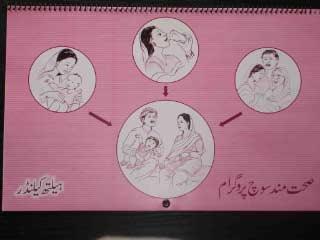
THP Materials (Training Manual, Training Video & Health Calendar)
Innovation Summary

 Perinatal depression affects 20-30% of women in low-income countries and is a risk factor for child development. The “Thinking Healthy Programme (THP)” based on cognitive behavioral therapy techniques, helped reduce perinatal depression in a low socioeconomic setting. [1, 2] It was delivered during pregnancy through the first postnatal year.
Perinatal depression affects 20-30% of women in low-income countries and is a risk factor for child development. The “Thinking Healthy Programme (THP)” based on cognitive behavioral therapy techniques, helped reduce perinatal depression in a low socioeconomic setting. [1, 2] It was delivered during pregnancy through the first postnatal year.
THP was delivered by non-mental health community based agents called Lady Health Workers of Pakistan. The program consisted of 16 home-based sessions: weekly in the last month of pregnancy, three sessions in the first month postnatal, and then once a month thereafter. Sessions involved use of empathic listening, guided discovery through use of pictures, and collaboration with the family to harness family support. The goal of the follow-up program is to examine if the intervention has longer term impacts on various cognitive, socio-emotional and physical outcomes in children now aged 7 years.
Gallery
Impact Summary
Thinking Healthy Programme (2008), Formative and Trial Phase
- 73% of mothers in the intervention vs 41% in the control recovered from depression, at 12 months post-partum.
- Women who took part in the THP intervention had higher levels of social support, better functioning; their infants had fewer episodes of diarrhea and better immunization coverage.
- Both parents in the intervention arm reported spending more time every day on play-related activities. [2]
Current Follow-up (Seven Years Later)
- Of the 964 mothers and 964 children in the original intervention, 884 mothers and 884 children have been re-enrolled and assessed.
- 300 mothers who were not depressed at the prenatal THP trial, and their children, have also been enrolled and assessed.
Innovation
In the Thinking Healthy Programme (THP), Lady Health Workers (LHWs) were trained to deliver a Cognitive Behavior Therapy (CBT) based intervention to depressed women, beginning in the last month of pregnancy and ending 12 months postpartum. The intervention is based in a psychosocial model and not presented as a ‘treatment’ for a ‘mental health problem’ but rather as way to improve positive and healthy thinking around the mother and the baby. The actual delivery of the intervention was fully integrated into the routine practice of existing community-based maternal and child health education efforts and is delivered in the woman’s home.
The intervention is delivered over 16 home visits and is divided into 5 modules: (1) preparing for the baby, (2) the baby’s arrival, (3) early infancy, (4) middle infancy, and (5) late infancy. Each of these modules is divided into three sections: (a) mother’s personal health, (b) mother’s relationship with baby, and (c) mother’s relationship with people around her. Within each module, each session that the LHW provides in the home employs a three-step approach that is carried throughout the program:
Step-1: Learning to identify unhealthy thinking: In order to promote healthy thinking, it is important to be aware of the common types of unhealthy or unhelpful thinking styles that gradually develop as a result of life problems or experiences.
Step-2: Learning to replace unhealthy thinking with healthy thinking: Identifying such unhealthy thinking styles enables mothers to examine how they feel and what actions they take when they think in this way. The program helps mothers question the accuracy of such thoughts and suggest alternative thoughts that are healthier.
Here the traditional CBT approach has been modified by involving the whole family in suggesting alternative healthy thinking. Thus they can assist the mother challenge and replace unhealthy thinking with healthy thinking.
Step-3: Practicing healthy thinking and acting: The program suggests activities and homework to help mothers to practice thinking and acting healthy. Carrying out these activities is essential for the success of the program.
Mothers receive health education and other materials tailored to their individual needs to help them progress between sessions. The focal point of these activities is a designated “health corner” that is established in each home, and a Mother and Child Health Calendar provided to each family. This calendar, consisting of pictorial and verbal key messages of each session, serves as a visual cue for the whole family to follow the program between sessions. In addition, the calendar has monitoring tools that help the mother chart her own progress, and that of her infant‘s, throughout the program. It is essential that the mother monitors herself and carries out the homework between sessions. The progress between sessions is discussed in the next session.
At the heart of the program delivery is the incorporation of CBT techniques (active listening, collaboration with the family, guided discovery of alternative beliefs and the assigning of homework to apply what had been learned) by the LHWs. It is also important for the training to be structured and standardized. As such, each of the 5 modules has a specially designed pictorial activity workbook that is used by the trainer to conduct a session with the mother. Each mother receives her own activity workbook where activities carried out in each session are noted.
Collaboration
Funders
- Thinking Healthy Programme (2008), Formative and Trial Phase
- Wellcome Trust (UK)
- Grand Challenges Canada (current follow-up)
Key Partners Involved in Current Follow-up
- Human Development Research Foundation (Pakistan)
- Duke University (USA)
- University of Liverpool (UK)
- University of Essex (UK)
Evaluation Methods
In the original intervention, mothers at 6 months post-partum and 12 months post-partum were assessed using the DSM-IV for major depressive episodes, through a randomized control trial. Infant health in both the intervention and control group was assessed by measuring stunting, exposure to exclusive breastfeeding, parent-reported time spent on play activities, and diarrheal episodes.
Seven years after the original program, the mother-child dyads who participated in the trial were re-enrolled. A comparison group of mother-child dyads from among women who were not depressed at the time of the original program was also enrolled. The two groups were compared on a variety of child cognitive, socio-emotional, and physical health outcomes.
The intervention’s impact on the children’s physical growth, cognition, language, and socioemotional capacity will be measured. In addition, the project team will collect extensive socio-emotional development data, including child anxiety symptoms, and family context such as harsh parenting, the home environment etc.
Finally, qualitative data will be collected through focus group discussions with the Lady Health Workers who provided the original THP intervention. This will help inform whether or not the THP intervention is sustainable.
References
- Rahman A. (2007) Challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan – a multi-method study. Arch Womens Ment Health 2007; 10: 211-9.
- Rahman A., et al. (2008) Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet 2008; 372(9642): 902-9.
Resources
-
Instruments & Batteries
-
ACER. Literacy.
-
Children’s color Trail Test - Executive Function.
-
Stroop like Day and Night Test – Executive Function.
-
Dimensional Change Card Sort - Executive Function.
-
SPENCE Children’s Anxiety Scale – Socio emotional.
-
Strength and Difficulties Questionnaire (SDQ) – Socio emotional.
-
Wechsler Preschool and Primary Scale of Intelligence (WPPSI) – Cognition.
-