In the randomized controlled trial assessing the efficacy of this intervention, the intervention was found to be associated with significant benefit to the mother-infant relationship. [1] At both six and 12 months post-partum, compared to control mothers, in directly observed, videotaped, interactions with their infants, mothers in the intervention group were significantly more sensitive (6 months: p<.05, d=0.24; 12 months: p<.05, d=0.25) and less intrusive (6 months: p<.05, d=0.25; 12 months: p<.05, d=0.24). [6] The intervention was also associated with a higher rate of secure infant attachments at 18 months (i.e. 74% versus 63%; Wald=4.74, OR=1.70, p<.05). [6] There was also a benefit of the intervention in terms of maternal depressed mood at six months. With regard to child cognitive outcome, infant functioning was assessed with the Bayley Scales of Development (Mental Development Index) at 18 months. There was some evidence for the benefit of the intervention in relation to this outcome, even at this early stage: the mean MDI scores for infants in the intervention group was 85.25 (SD 10.87), while for the controls it was 83.10 (9.96), (F(261)=2.82, p = .094). When the level of family adversity was taken into account, this effect was found to be strengthened for those with less extreme family adversity: thus, for families experiencing less extreme adversity, the mean MDI score was 87.27 (11.16) in the intervention group, vs. 82.72 (10.72) in the control group (F(1,259)=4.98, p=.03).
At present, the intervention is being evaluated by assessing the long term impact on cognitive and socio-emotional development in the children who participated in the original project. Thirteen years later, 75% of the original sample, has been re-recruited and a range of systematic standardized assessments have been completed to measure child cognitive functioning, school attainment, child emotional/behavioral functioning, the home environment, child health and growth, family functioning, as well as neural functions implicated in self-regulation (e.g. inhibitory control, self-monitoring, and working memory) and the stress response (e.g. cortisol secretion). In addition, data has been collected from mothers on a range of other child and maternal outcomes. The project team is currently in the process of analyzing these data.
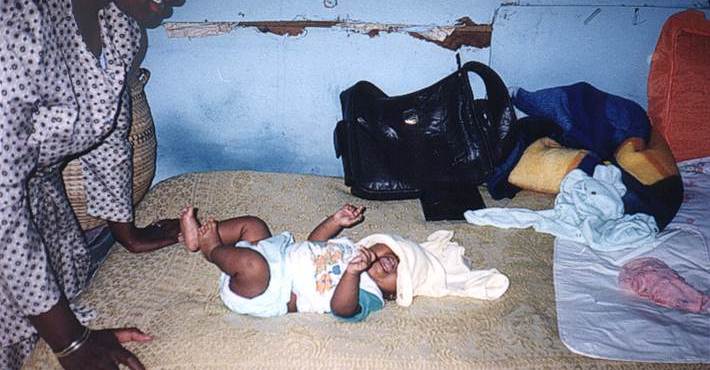
 Saving Brains and unlocking human potential depends on reliable parental care that is sensitive to the developmental needs of children. In the context of poverty and high adversity the capacity of parents to provide the kind of care that promotes good child developmental outcome can be severely compromised. There is emerging evidence that sensitive maternal care and associated secure infant attachment are strong predictors of a range of child developmental outcomes, including child growth and physical health status, child cognitive development, and socio-emotional functioning.
Saving Brains and unlocking human potential depends on reliable parental care that is sensitive to the developmental needs of children. In the context of poverty and high adversity the capacity of parents to provide the kind of care that promotes good child developmental outcome can be severely compromised. There is emerging evidence that sensitive maternal care and associated secure infant attachment are strong predictors of a range of child developmental outcomes, including child growth and physical health status, child cognitive development, and socio-emotional functioning.